Nociceptors: All about Pain Receptors


Written and verified by the psychologist Valeria Sabater
We all experience pain. Sometimes, even our own organism causes pain by triggering inflammation. Now, although we all feel pain, we’re not well-informed on the sensory neurons that are involved in it. In this article, we’ll be talking about nociceptors, the pain receptors.
All human beings (and all other living beings with a central nervous system) would love nothing more than not feel any pain. However, believe it or not, experiencing pain is key in life. If we were immune to burns, injuries, or the physical indicators of a disease, we’d most likely lead really short lives. Moreover, it’s known that people with congenital analgesia (insensitivity to pain) live tragic and short lives.
Pain is like a warning and helps us react to dangerous or harmful stimuli. Thus, we could say that nociceptors guarantee our survival since they allow us to have a better quality of life and relate much better to ourselves and our environment.

Nociceptors
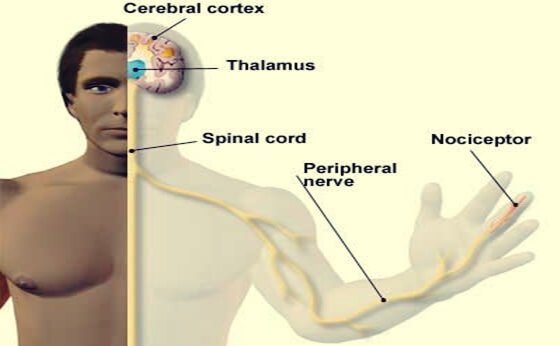
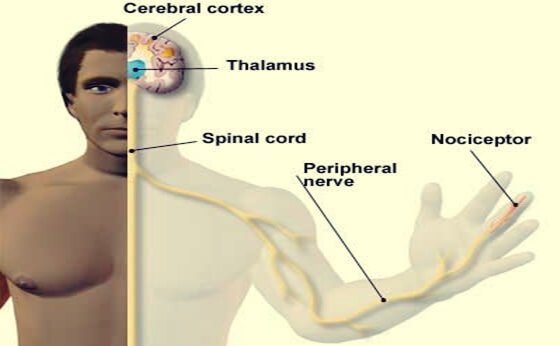
As previously mentioned, pain is necessary and we can’t live without it. But what makes us experience it, biologically speaking? We can say that the brain’s pain receptors are the only culprits. However, they do need the help of a few allies that detect painful stimuli and of a complex network that transmits the information of that experience, such as the thalamus and the afferent nerve fibers.
Moreover, nociceptors are in charge of detecting these unpleasant sensations. They’re nerve endings (the end of axons) that are located throughout the body. They’re found both in our external tissues (skin) and in any area of our internal physiology (muscles, intestines, bladder, ovaries, etc.). They assess the body’s damage while we’re experiencing pain. In other words, they’re in charge of transmitting that information to the central nervous system.
It’s important to note that humans and animals aren’t the only living beings that have these sensory receptors. Some of the simplest organisms have nociceptive functions. We all need these structures to survive.
Types of nociceptors
Here are the types of nociceptors we have in our body:
- Chemoreceptors react to certain chemicals that our tissues release in the face of an infection, inflammation, or disease. These are substances such as bradykinin and histamine that reach the blood when we suffer an injury, when a cut gets infected, or when we suffer from a blow.
- Thermoreceptors are the pain receptors that activate when we come into contact with a surface or an element of a very high temperature. We often experience this painful sensation without even knowing what happened or what we touched.
- Mechanoreceptors are activated by any mechanical pressure that can injure the individual or deform bodily tissue. This is the most common type of pain and the fastest we notice since this information passes through Aδ fibers.
- Silent nociceptors take a long time to activate. They’re located in inflamed tissues, right next to an injury.
- Polymodal nociceptors are a challenge for scientists because they respond to every type of stimuli we mentioned above.

Why does pain turn chronic?
What do we know thus far about nociceptors? One, that they’re located at the end of axons, and two, that they react to dangerous thermal, mechanical, or chemical stimuli. Now, we also know that certain types of pain are more bearable than others and that some conditions make pain become chronic.
Some experts establish that pain is proportionate to the severity of the injury or dysfunction. If you cut your finger, for example, your pain won’t last for more than 2 or 3 days as long as you clean and treat the wound properly. However, burns are different. Severe injuries like this one damage more tissue, which complicates the healing process a lot more.
On the other hand, it’s also important to differentiate nociceptive pain from neuropathic pain. The first one is produced by mechanical, thermal, or chemical stimuli. Neuropathic pain, however, involves damage to the nervous system. There may be a small neurological alteration that would make those axons or pain receptors react more intensely and enduringly to any stimulus. The latter is related to debilitating conditions such as fibromyalgia.
Science is facing the challenge of developing more refined and personalized drugs, chemical agents that act on those concrete pain receptors that trigger pain, so that it no longer affects the quality of life of those suffering from serious injuries or conditions.
We all experience pain. Sometimes, even our own organism causes pain by triggering inflammation. Now, although we all feel pain, we’re not well-informed on the sensory neurons that are involved in it. In this article, we’ll be talking about nociceptors, the pain receptors.
All human beings (and all other living beings with a central nervous system) would love nothing more than not feel any pain. However, believe it or not, experiencing pain is key in life. If we were immune to burns, injuries, or the physical indicators of a disease, we’d most likely lead really short lives. Moreover, it’s known that people with congenital analgesia (insensitivity to pain) live tragic and short lives.
Pain is like a warning and helps us react to dangerous or harmful stimuli. Thus, we could say that nociceptors guarantee our survival since they allow us to have a better quality of life and relate much better to ourselves and our environment.

Nociceptors
As previously mentioned, pain is necessary and we can’t live without it. But what makes us experience it, biologically speaking? We can say that the brain’s pain receptors are the only culprits. However, they do need the help of a few allies that detect painful stimuli and of a complex network that transmits the information of that experience, such as the thalamus and the afferent nerve fibers.
Moreover, nociceptors are in charge of detecting these unpleasant sensations. They’re nerve endings (the end of axons) that are located throughout the body. They’re found both in our external tissues (skin) and in any area of our internal physiology (muscles, intestines, bladder, ovaries, etc.). They assess the body’s damage while we’re experiencing pain. In other words, they’re in charge of transmitting that information to the central nervous system.
It’s important to note that humans and animals aren’t the only living beings that have these sensory receptors. Some of the simplest organisms have nociceptive functions. We all need these structures to survive.
Types of nociceptors
Here are the types of nociceptors we have in our body:
- Chemoreceptors react to certain chemicals that our tissues release in the face of an infection, inflammation, or disease. These are substances such as bradykinin and histamine that reach the blood when we suffer an injury, when a cut gets infected, or when we suffer from a blow.
- Thermoreceptors are the pain receptors that activate when we come into contact with a surface or an element of a very high temperature. We often experience this painful sensation without even knowing what happened or what we touched.
- Mechanoreceptors are activated by any mechanical pressure that can injure the individual or deform bodily tissue. This is the most common type of pain and the fastest we notice since this information passes through Aδ fibers.
- Silent nociceptors take a long time to activate. They’re located in inflamed tissues, right next to an injury.
- Polymodal nociceptors are a challenge for scientists because they respond to every type of stimuli we mentioned above.

Why does pain turn chronic?
What do we know thus far about nociceptors? One, that they’re located at the end of axons, and two, that they react to dangerous thermal, mechanical, or chemical stimuli. Now, we also know that certain types of pain are more bearable than others and that some conditions make pain become chronic.
Some experts establish that pain is proportionate to the severity of the injury or dysfunction. If you cut your finger, for example, your pain won’t last for more than 2 or 3 days as long as you clean and treat the wound properly. However, burns are different. Severe injuries like this one damage more tissue, which complicates the healing process a lot more.
On the other hand, it’s also important to differentiate nociceptive pain from neuropathic pain. The first one is produced by mechanical, thermal, or chemical stimuli. Neuropathic pain, however, involves damage to the nervous system. There may be a small neurological alteration that would make those axons or pain receptors react more intensely and enduringly to any stimulus. The latter is related to debilitating conditions such as fibromyalgia.
Science is facing the challenge of developing more refined and personalized drugs, chemical agents that act on those concrete pain receptors that trigger pain, so that it no longer affects the quality of life of those suffering from serious injuries or conditions.
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.







