Mad Cow Disease or Spongiform Encephalopathy

Mad cow disease or spongiform encephalopathy is a lesser-known but equally important type of dementia. Generally, when you hear the word dementia, you tend to think of Alzheimer’s disease. However, many other types of dementia affect thousands of people.
Firstly, let’s delve a little deeper into dementia, which is a multi-etiological disease that involves the onset of intellectual impairment. Not all types of dementia are irreversible or progressive. However, intellectual impairment usually affects the individual’s ability to carry out their day-to-day activities.
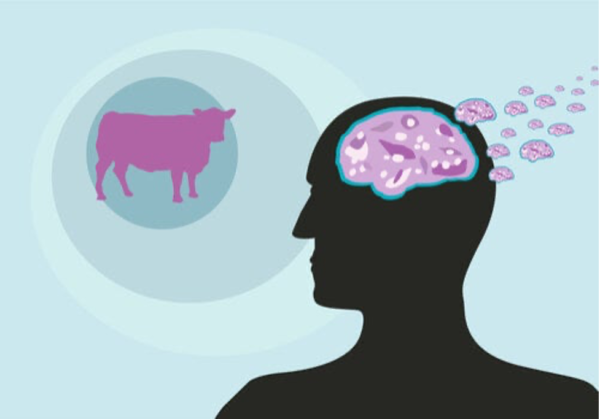
Spongiform encephalopathy, also known as mad cow disease or Creutzfeldt-Jakob disease (CJD), is an infectious type of dementia caused by prions. It’s a degenerative disease and it appears spontaneously or due to genetic inheritance. It affects one to two per 10,000 people (Vich, 2006).
Causes of mad cow disease
As we mentioned above, mad cow disease (spongiform encephalopathy) is infectious. It’s caused by prions. A prion is an altered or poorly formed protein that can modify similar proteins in the body, leading to infections.
The incubation period of the disease can be quite long. However, once the patient notices symptoms, the disease tends to progress very fast. Furthermore, almost 90% of cases are fatal.
This protein affects the brain and the nervous system. Holes form in the brain, making it look like a sponge. This is where the term “spongiform” comes from. Although experts don’t know for certain, they believe people can catch it in three different ways (Vich, 2006):
- Eating bovine animals infected with the disease.
- Genetic. In autosomal dominant fashion, as there’s a mutation in the gene that encodes the prion protein.
- Occasionally, of iatrogenic origin.
“Medical science has made such tremendous progress that there’s hardly a healthy human left.“
-Aldous Leonard Huxley-
Symptoms of mad cow disease
People with mad cow disease might suffer from the following symptoms:
- Depression. Sadness, anhedonia, fear of being a burden, lack of hope, etc. Consequently, the patient suffers significant discomfort and is unable to function.
- Delirium. Mental confusion and false awareness of reality. Kraepelin defines delirium as a cognitive distortion that suddenly occurs due to a pathological cause.
- Hallucinations. Patients falsely perceive objects and events. They affect the senses. For example, the person feels, smells, and hears something that isn’t really there or isn’t happening. Esquirol defined hallucinations as “When a person fully believes they’ve perceived a sensation when no external object has impressed the senses”.
- Ataxia. Loss of coordination, clumsiness, and stiffness.
- Memory loss.
- Difficulty speaking.
- Difficulty swallowing
- Dementia.

Prevention
There’s no treatment for this disease, as is the case with other illnesses that manifest themselves in the form of dementia. Consequently, authorities suggest preventive measures:
- Active and passive surveillance methods. This way, affected animals can be rapidly detected on both farms and slaughterhouses.
- Prohibition of meat and bone meal from mammals. In addition, processed animal proteins shouldn’t be fed to animals intended for human consumption.
- Veterinary inspections on livestock farms. Furthermore, it’s advisable to monitor farms for plagues.
- Putting potentially infected animals to sleep.
- Not consuming meat of suspicious origin.
However, if there’s a suspicion of an outbreak or any doubts about the disease, a professional should always be consulted. Health professionals are the only people who can give a reliable diagnosis and advice on what measures should be taken.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Beteta, E. (2004). Neuropatología de las demencias. Revista de neuro-psiquiatría, 67, 80-105.
- Cassany, D., & Martí, J. (1998). Estrategias divulgativas del concepto prión. Quark, (12), 58-66.
- Olazarán-Rodríguez, J., Agüera-Ortiz, L. F., & Muñiz-Schwochert, R. (2012). Síntomas psicológicos y conductuales de la demencia: prevención, diagnóstico y tratamiento. Rev Neurol, 55(10), 598-608.
- Vich, F. D. A. B. (2006). Encefalopatía espongiforme bovina: el” mal de las vacas locas”. Revista de administración sanitaria siglo XXI, 4(4), 655-673.
- Zaninovic, V., & Dueñas, A. (2016). Demencia viral transmisible. Confirmación de un caso de enfermedad de Creutzfeldt-Jakob. Colombia Médica, 14(1), 40-42.
- Zúñiga-Quiñónez, S., Urista-Vidrio, M. C., & Ruiz-Sandoval, J. L. (2002). Enfermedad de Creutzfeldt Jacob. Del kuru a las vacas locas. Revista Mexicana de Neurociencia, 3(1), 13-19.
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








