The Neurobiology of Trauma

Today, child abuse is considered a public health problem. That’s why, from the past few decades, experts have been trying to understand the effects of exposure to traumatic life experiences on children’s psychopathology. That, however, raises another important question: how does trauma neurobiology develop?
In recent years, clinical research has focused on explaining the impact of traumatic, one-time events as well as exposure to neglect and chronic abuse. Different studies have shown that isolated traumatic events tend to produce responses conditioned by the memories of the event.
Meanwhile, chronic abuse or recurring exposure to traumatic events, such as exposure to repeated medical or surgical procedures, also seem to have generalized effects on neurobiological development (1). It would seem that a variety of factors contribute to the severity of the psychological damage that trauma causes to an individual’s neurobiology:
- The child’s age when they were first traumatized.
- The frequency of traumatic experiences.
- To what degree the caretakers contribute to the traumatic nature of the event.
We know that traumatic events can change brain structures. Also, they compromise emotional, cognitive, and body function, which weakens patients. However, specialists still don’t have a good understanding of the neurobiology of trauma and, in spite of its prevalence, there aren’t many available educational resources (2).
In 2013, the American Psychiatric Association revised the diagnostic criteria for post-traumatic stress disorder (PTSD) in the Diagnostic and Statistical Manual of Mental Disorders. They added a new category to the manual: disorders related to trauma and stress.

Post-traumatic stress disorder
Traumatic events can negatively affect emotional, cognitive, and bodily functions. That, in turn, can cause debilitating symptoms for patients (3, 4), and a PTSD diagnosis. The trauma that causes PTSD can happen either:
- During a one-time event. For example, being a witness to gender violence.
- Over a prolonged period of time. For example, chronic child abuse.
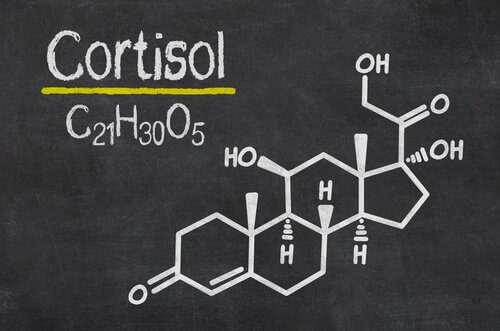
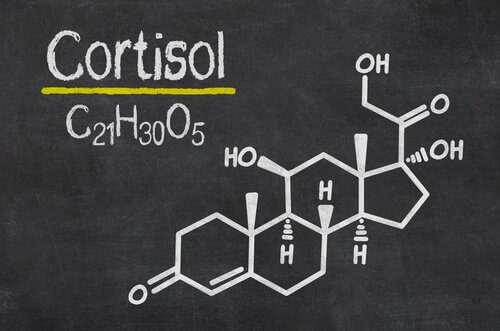
Significant stress causes the hippocampus (involved in memory processing) and the amygdala (involved in emotional processing) to be flooded with the stress hormone cortisol (3). The individual can’t process the traumatic experience as something that’s over (though the threat doesn’t exist that way anymore) and the memory remains active in the brain (2).
That’s why PTSD symptoms can come up a long time after the traumatic event. In fact, about 25% of people with PTSD start to experience symptoms much later (5).
The neurobiology of trauma: affected areas
The neurobiological changes that happen with trauma and vary from normal development include areas involved in homeostasis regulation. They are (6, 7):
- The encephalic trunk and the locus coeruleus.
- Memory systems (including the hippocampus, the amygdala, and the frontal cortex).
- The areas of the brain involved in executive functions:
- Orbitofrontal cortex.
- Cingulate cortex.
- Dorsolateral prefrontal cortex.
- The neuroendocrine system, including:
- The hypothalamic, pituitary, adrenal axis (HPA).
- All conceivable neurotransmitter systems.
The brainstem and the mesencephalon
The brain systems that respond to threats are the sympathetic and parasympathetic nervous systems. They both originate in the brainstem. Thus, early exposure to extreme threats and inappropriate care has a significant and long-term impact on the body’s ability to modulate the sympathetic and parasympathetic systems in response to threats (16).
Catecholamines
Some studies show that children who suffer from PTSD or have been abused have significantly higher concentrations of dopamine and norepinephrine than test subjects who haven’t experienced abuse (18, 19).
Rate of cardiac variability
Children who have suffered trauma have less heart rate variability than healthy subjects (20).
Cortisol
In general (and in contrast to cortisol studies of adults with PTSD), children with a history of trauma show significantly higher cortisol levels than subjects in the control group.
The limbic system
Studies show that when adults with PTSD remember their trauma, they have elevated activity in the right amygdala. In the study, lower activation in the speech centers of the brain accompanied the elevated amygdala activity (22).
The hippocampus
It’s interesting to note that both trauma and PTSD can actually reduce the hippocampal volume in some individuals. As a consequence of these findings, Davidson and his collaborators have proposed that the impact of hippocampal participation in psychopathology can be more evident in the processing of emotional information. Therefore, children with hippocampal damage might be more likely to display emotional behavior in inappropriate contexts (23).
Other areas affected by trauma are:
- The pre-frontal cortex.
- Hemispheric lateralization.
- The cerebellum, the corpus callosum, and the area of the brain responsible for integrating experiences.
The long-term effects of neurobiological deregulation due to trauma
Loss of emotional self-regulation
Chronic trauma in children can lead to a lack of emotional self-regulation. This lack of emotional regulation processes can lead to problems with children’s sense of self. This manifests itself in the following problems (8, 9):
- Lack of a continuous and predictable sense of self and a bad sense of separation and body image alterations.
- Affect modulation deficiency and problems with impulse control. Aggression towards self and others can also be a problem.
- Uncertainty about other people’s trustworthiness. That can lead to mistrust and intimacy problems.
Learning and memory
Some characteristics of children who have experienced trauma are:
- A tendency towards hypervigilance. They worry about imminent danger and tend to attack ambiguous stimuli (10).
- Unsurprisingly, this affects the way that children with trauma organize their perceptions of the world. It’s also associated with generalized learning problems and academic performance (11).
- Limitations in the attention they give to threatening stimuli. Children with PTSD might display indifference to things that other children find challenging or stimulating.
- Paranoid ideas and mistaken perceptions are also common (12, 13).
Social problems
Exposure to violence also causes social problems in children:
- They often have trouble behaving in a socially appropriate way (14).
- As a result, they’re frequently out of synch with other people. During elementary school, they often give the impression that they have an intellectual disability (15).

Physical illness
Other studies show that traumatized children are vulnerable to a whole host of physical illnesses. Similar to adults, they’re 10% to 15% more likely to suffer from cancer, heart problems, and diabetes.
During adolescence, they often engage in destructive behaviors towards themselves and others. They’re also approximately 300% more likely to have a drug abuse problem, engage in self-harm, or behave aggressively towards others (16) than their peers who haven’t suffered from trauma.
Trauma also makes it difficult for children to express what they’re going through with words. Instead, they see the world as a place fraught with dangers, which activates neurobiological systems designed for human survival, even when they’re in objectively safe situations. Thus, while children can’t talk about their traumatic experiences, their trauma will probably be expressed as an incarnation of what happened to them.
Consequently, the goal of therapy for children who have experienced trauma is to help them develop a sense of physical control. Therapists also need to stimulate their awareness of who they are and what happened to them. That way, they’ll be able to understand what’s happening in the present and stop recreating their traumatic past on emotional, behavioral, and biological levels.
Today, child abuse is considered a public health problem. That’s why, from the past few decades, experts have been trying to understand the effects of exposure to traumatic life experiences on children’s psychopathology. That, however, raises another important question: how does trauma neurobiology develop?
In recent years, clinical research has focused on explaining the impact of traumatic, one-time events as well as exposure to neglect and chronic abuse. Different studies have shown that isolated traumatic events tend to produce responses conditioned by the memories of the event.
Meanwhile, chronic abuse or recurring exposure to traumatic events, such as exposure to repeated medical or surgical procedures, also seem to have generalized effects on neurobiological development (1). It would seem that a variety of factors contribute to the severity of the psychological damage that trauma causes to an individual’s neurobiology:
- The child’s age when they were first traumatized.
- The frequency of traumatic experiences.
- To what degree the caretakers contribute to the traumatic nature of the event.
We know that traumatic events can change brain structures. Also, they compromise emotional, cognitive, and body function, which weakens patients. However, specialists still don’t have a good understanding of the neurobiology of trauma and, in spite of its prevalence, there aren’t many available educational resources (2).
In 2013, the American Psychiatric Association revised the diagnostic criteria for post-traumatic stress disorder (PTSD) in the Diagnostic and Statistical Manual of Mental Disorders. They added a new category to the manual: disorders related to trauma and stress.

Post-traumatic stress disorder
Traumatic events can negatively affect emotional, cognitive, and bodily functions. That, in turn, can cause debilitating symptoms for patients (3, 4), and a PTSD diagnosis. The trauma that causes PTSD can happen either:
- During a one-time event. For example, being a witness to gender violence.
- Over a prolonged period of time. For example, chronic child abuse.
Significant stress causes the hippocampus (involved in memory processing) and the amygdala (involved in emotional processing) to be flooded with the stress hormone cortisol (3). The individual can’t process the traumatic experience as something that’s over (though the threat doesn’t exist that way anymore) and the memory remains active in the brain (2).
That’s why PTSD symptoms can come up a long time after the traumatic event. In fact, about 25% of people with PTSD start to experience symptoms much later (5).
The neurobiology of trauma: affected areas
The neurobiological changes that happen with trauma and vary from normal development include areas involved in homeostasis regulation. They are (6, 7):
- The encephalic trunk and the locus coeruleus.
- Memory systems (including the hippocampus, the amygdala, and the frontal cortex).
- The areas of the brain involved in executive functions:
- Orbitofrontal cortex.
- Cingulate cortex.
- Dorsolateral prefrontal cortex.
- The neuroendocrine system, including:
- The hypothalamic, pituitary, adrenal axis (HPA).
- All conceivable neurotransmitter systems.
The brainstem and the mesencephalon
The brain systems that respond to threats are the sympathetic and parasympathetic nervous systems. They both originate in the brainstem. Thus, early exposure to extreme threats and inappropriate care has a significant and long-term impact on the body’s ability to modulate the sympathetic and parasympathetic systems in response to threats (16).
Catecholamines
Some studies show that children who suffer from PTSD or have been abused have significantly higher concentrations of dopamine and norepinephrine than test subjects who haven’t experienced abuse (18, 19).
Rate of cardiac variability
Children who have suffered trauma have less heart rate variability than healthy subjects (20).
Cortisol
In general (and in contrast to cortisol studies of adults with PTSD), children with a history of trauma show significantly higher cortisol levels than subjects in the control group.
The limbic system
Studies show that when adults with PTSD remember their trauma, they have elevated activity in the right amygdala. In the study, lower activation in the speech centers of the brain accompanied the elevated amygdala activity (22).
The hippocampus
It’s interesting to note that both trauma and PTSD can actually reduce the hippocampal volume in some individuals. As a consequence of these findings, Davidson and his collaborators have proposed that the impact of hippocampal participation in psychopathology can be more evident in the processing of emotional information. Therefore, children with hippocampal damage might be more likely to display emotional behavior in inappropriate contexts (23).
Other areas affected by trauma are:
- The pre-frontal cortex.
- Hemispheric lateralization.
- The cerebellum, the corpus callosum, and the area of the brain responsible for integrating experiences.
The long-term effects of neurobiological deregulation due to trauma
Loss of emotional self-regulation
Chronic trauma in children can lead to a lack of emotional self-regulation. This lack of emotional regulation processes can lead to problems with children’s sense of self. This manifests itself in the following problems (8, 9):
- Lack of a continuous and predictable sense of self and a bad sense of separation and body image alterations.
- Affect modulation deficiency and problems with impulse control. Aggression towards self and others can also be a problem.
- Uncertainty about other people’s trustworthiness. That can lead to mistrust and intimacy problems.
Learning and memory
Some characteristics of children who have experienced trauma are:
- A tendency towards hypervigilance. They worry about imminent danger and tend to attack ambiguous stimuli (10).
- Unsurprisingly, this affects the way that children with trauma organize their perceptions of the world. It’s also associated with generalized learning problems and academic performance (11).
- Limitations in the attention they give to threatening stimuli. Children with PTSD might display indifference to things that other children find challenging or stimulating.
- Paranoid ideas and mistaken perceptions are also common (12, 13).
Social problems
Exposure to violence also causes social problems in children:
- They often have trouble behaving in a socially appropriate way (14).
- As a result, they’re frequently out of synch with other people. During elementary school, they often give the impression that they have an intellectual disability (15).

Physical illness
Other studies show that traumatized children are vulnerable to a whole host of physical illnesses. Similar to adults, they’re 10% to 15% more likely to suffer from cancer, heart problems, and diabetes.
During adolescence, they often engage in destructive behaviors towards themselves and others. They’re also approximately 300% more likely to have a drug abuse problem, engage in self-harm, or behave aggressively towards others (16) than their peers who haven’t suffered from trauma.
Trauma also makes it difficult for children to express what they’re going through with words. Instead, they see the world as a place fraught with dangers, which activates neurobiological systems designed for human survival, even when they’re in objectively safe situations. Thus, while children can’t talk about their traumatic experiences, their trauma will probably be expressed as an incarnation of what happened to them.
Consequently, the goal of therapy for children who have experienced trauma is to help them develop a sense of physical control. Therapists also need to stimulate their awareness of who they are and what happened to them. That way, they’ll be able to understand what’s happening in the present and stop recreating their traumatic past on emotional, behavioral, and biological levels.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
-
van der Kolk, B. A. (2003). The neurobiology of childhood trauma and abuse. Child and adolescent psychiatric clinics of North America, 12(2), 293-318.
-
Kim, S., Lax, L., Ross, D., Ng, D., Grossi, D., Gupta, R., … & Taylor, V. (2017). Visualizing the Neurobiology of Trauma: Design and evaluation of an eLearning module for continuing professional development of family physicians in the Online Psychiatric Education Network. Journal of Biocommunication, 41(2).
-
Heim, C., & Nemeroff, C. B. (2009). Neurobiology of posttraumatic stress disorder. CNS spectr, 14(1 Suppl 1), 13-24.
-
Sherin, J. E., & Nemeroff, C. B. (2011). Post-traumatic stress disorder: the neurobiological impact of psychological trauma. Dialogues in clinical neuroscience, 13(3), 263.
-
Sareen, J. (2014). Posttraumatic stress disorder in adults: impact, comorbidity, risk factors, and treatment. The Canadian Journal of Psychiatry, 59(9), 460-467.
-
Wiener, S. G., Lowe, E. L., & Levine, S. (1992). Pituitary-adrenal response to weaning in infant squirrel monkeys. Psychobiology, 20(1), 65-70.
-
Stanton, M. E., Gutierrez, Y. R., & Levine, S. (1988). Maternal deprivation potentiates pituitary-adrenal stress responses in infant rats. Behavioral neuroscience, 102(5), 692.
-
Kolk, B. A., & Fisler, R. E. (1994). Childhood abuse and neglect and loss of self-regulation. Bulletin of the Menninger Clinic, 58(2), 145.
-
Cole, P. M., & Putnam, F. W. (1992). Effect of incest on self and social functioning: A developmental psychopathology perspective. Journal of consulting and clinical psychology, 60(2), 174.
-
Dodge, K. A., & Price, J. M. (1994). On the relation between social information processing and socially competent behavior in early school‐aged children. Child development, 65(5), 1385-1397.
-
Cicchetti, D., Toth, S. L., & Hennessy, K. (1989). Research on the consequences of child maltreatment and its application to educational settings. Topics in Early Childhood Special Education, 9(2), 33-55.
-
Lewis, D. O., Shanok, S. S., Pincus, J. H., & Glaser, G. H. (1979). Violent juvenile delinquents: Psychiatric, neurological, psychological, and abuse factors. Journal of the American Academy of Child & Adolescent Psychiatry, 18(2), 307-319.
-
Lewis, D. O., Pincus, J. H., Feldman, M., Jackson, L., & Bard, B. (1986). Psychiatric, neurological, and psychoeducational characteristics of 15 death row inmates in the United States. American journal of psychiatry, 143(7), 838-845.
-
Weinberg, M. K., & Tronick, E. Z. (1998). The impact of maternal psychiatric illness on infant development. The Journal of clinical psychiatry.
-
Erickson, M. F., & Egeland, B. (2002). Child neglect. The APSAC handbook on child maltreatment, 2, 3-20.
-
Felitti, V., Anda, R., & Nordernbeg, D. (1998). Relationship of childhood abuse to many of the leading causes of death in adults: The adverse childhood experiences study. Journal of Psychiatry, 163, 245-258.
-
Pitman, R. K. (1989). Post-traumatic stress disorder, hormones, and memory. Biological psychiatry, 26(3), 221-223.
-
De Bellis, M. D., Baum, A. S., Birmaher, B., Keshavan, M. S., Eccard, C. H., Boring, A. M., … & Ryan, N. D. (1999). Developmental traumatology part I: biological stress systems∗. Biological psychiatry, 45(10), 1259-1270.
-
De Bellis, M. D., Keshavan, M. S., Clark, D. B., Casey, B. J., Giedd, J. N., Boring, A. M., … & Ryan, N. D. (1999). Developmental traumatology part II: brain development∗. Biological psychiatry, 45(10), 1271-1284.
-
Cohen, J. A., Perel, J. M., DeBellis, M. D., Friedman, M. J., & Putnam, F. W. (2002). Treating traumatized children: Clinical implications of the psychobiology of posttraumatic stress disorder. Trauma, Violence, & Abuse, 3(2), 91-108.
-
Hart, J., Gunnar, M., & Cicchetti, D. (1996). Altered neuroendocrine activity in maltreated children related to symptoms of depression. Development and Psychopathology, 8(1), 201-214.
-
Rauch, S. L., van der Kolk, B. A., Fisler, R. E., Alpert, N. M., Orr, S. P., Savage, C. R., … & Pitman, R. K. (1996). A symptom provocation study of posttraumatic stress disorder using positron emission tomography and script-driven imagery. Archives of general psychiatry, 53(5), 380-387.
-
Davidson, R. J., Jackson, D. C., & Kalin, N. H. (2000). Emotion, plasticity, context, and regulation: perspectives from affective neuroscience. Psychological bulletin, 126(6), 890.
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.







