Drugs and Mental Illness: What's the Connection?

The use of drugs results in many deaths every year. The UN did a global report in 2017 about drug consumption. It confirmed that, in the past year alone, drug-related deaths had risen by 11.4%.
The pleasant effects produced in the brain, which inhibit our reward centers, turn users into addicts. Prolonged consumption can lead to the degeneration of the neurons, affecting motivation, emotion, cognition, and executive control. All of this can sometimes produce a mental illness.
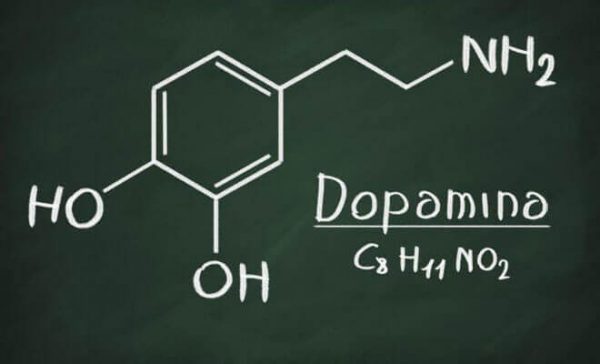
Drugs and their relation to dopamine
Dopamine is a neurotransmitter emitted by the brain. Its most important function has to do with feelings of pleasure. When we realize we like something, our brain releases dopamine, giving us a pleasant sensation. This way, our body tends to search for ways to generate those good sensations again.
Food and sex are two things that release dopamine. Drugs are another. All of these things release high quantities of dopamine in very particular areas, such as the nucleus accumbens. This area is central in the brain’s reward system and the integration of motivation and action. It maintains elevated connections with the limbic system and hippocampus.
How do drugs affect the brain?
Neurons are the nervous system’s cells in charge of reception, transformation, gestures, and information storage. There’s an area called the synaptic space between neurons. This space is very important for releasing neurotransmitters that make our internal chemical communication possible. After release, dopamine heads towards the synaptic space.
This means that, whenever we consume anything that could create addiction, it increases the dopamine levels in this synaptic space. Drugs may also partially block the re-uptake of the dopamine in that space, causing the same result. In both ways, higher dopamine levels in the synaptic space generate pleasant feelings or even euphoria.
Essentially, drugs have the same physiological effect as any natural intensifier, such as an exciting chat with a close friend. The problem is that the intensity of the effect is so much greater that natural highs end up feeling underwhelming in comparison after having felt the intense sensations of a drug. That’s where the drug becomes especially attractive.
Theories about dopamine and drugs
Some hypotheses have emerged, some without a lot of research to back them up, that talk about a deficit of dopamine levels, whether from natural causes or a lack of intensifiers coming from the centers that control our pleasure and well-being. According to the studies, this lack might predispose you to drug use.
In this case, if a person’s body isn’t releasing enough dopamine naturally, they could end up abusing activities that achieve the same feel-good effects. However, we can’t forget that this is still just a theory that needs a lot of empirical evidence to support it.
Mental illness
As we mentioned at the start of the article, drug use can be a slippery slope that leads to temporary or permanent mental problems.
The DSM-V recognizes intoxication, substance abuse, and withdrawal as disorders. However, there are other types of mental disorders that can be induced by these substances. Some appear more frequently than others, while some emerge under specific conditions. The most characteristic issues are psychotic disorders, bipolar disorder, depression, and anxiety. They all can manifest themselves not just in the moment of intoxication (i.e. the drug’s immediate effect) but also during withdrawal. At times, some drugs can even produce behavior on the schizophrenia spectrum.
Psychotic disorders are characterized by an alteration in the cognitive functions of the brain. This can even lead to a loss of intellectual capacity. Such anomalies in cognitive functions can fall into different categories.

Alterations in perception
- Hallucinations: seeing objects that don’t really exist (spaceships, etc.)
- Delusions: an object does exist, but it appears deformed (thinking that a real person is the devil in disguise)
- Paranoias: also known as Ekbom Syndrome, drug users may experience ectoparasitosis, or the sensation that insects like ants are covering the body. The anguish this produces can provoke drastic decisions, like trying to remove them through whatever means necessary (knives, scissors, etc.)
Alterations in thought
There are two categories of drug-induced alteration of thought:
- Loss of attention and associative capacity: a person with this symptom tends to be incapable of sorting through the stimuli they receive. When we talk to someone, we notice different stimuli: other voices, passing cars, lights from background commercials. People without these sensors are only capable of holding on to the information they want to. However, someone with this kind of thought-alteration doesn’t just transmit what they want. They may also bring up these background stimuli in the conversation.
- Delirious ideas: They imagine things that aren’t real. These thoughts may carry vestiges of truth. It may be something that could happen in real life. For example, the person becomes convinced their partner is cheating on them, and they envision their actual partner with an actual friend of theirs. However, the content of the delusion lacks organization. It’s totally illogical – imagining stalkers, crazy jealousy, etc.
Drugs produce unusual effects that are sometimes devastating. They don’t only cause harm to the physical body but also can produce serious mental issues. Treatment must be individualized according to the specific pathology each patient is suffering from. The treatment should also keep in mind their social circumstances, environments, and psychobiology.
Bibliographical references
Gil-Verona, J.A., Pastor, J.F., de Paz, F., Barbosa, M., Macias-Fernández, J.A., Maniega, M.A., Rami-Gonzalez, L., and Cañizares-Alejos, S. (2003). Neurologia de la adicción a la drogas de abuso. Revista de Neurologia, 36(4), 361-365.
American Psychiatry Association, (2014), Diagnostic and Statistical Manual of Mental Disorders., Washington, DC: United States, American Psychiatry Publishing.
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








