The Psychological Aspects of Dysautonomia


Written and verified by the psychologist Elena Sanz
Dysautonomia is a common condition, but it’s difficult to diagnose. Those who suffer from it experience dizziness, fatigue, tachycardia, headaches, and even fainting, yet they’re not always taken seriously. However, these symptoms have a significant impact on their quality of life. For this reason, it’s important to consider the psychological aspects of dysautonomia.
Although you may not have heard of this condition, it’s estimated that it affects one in one hundred people. Therefore, worldwide, around 70 million people would suffer from it.
Dysautonomia
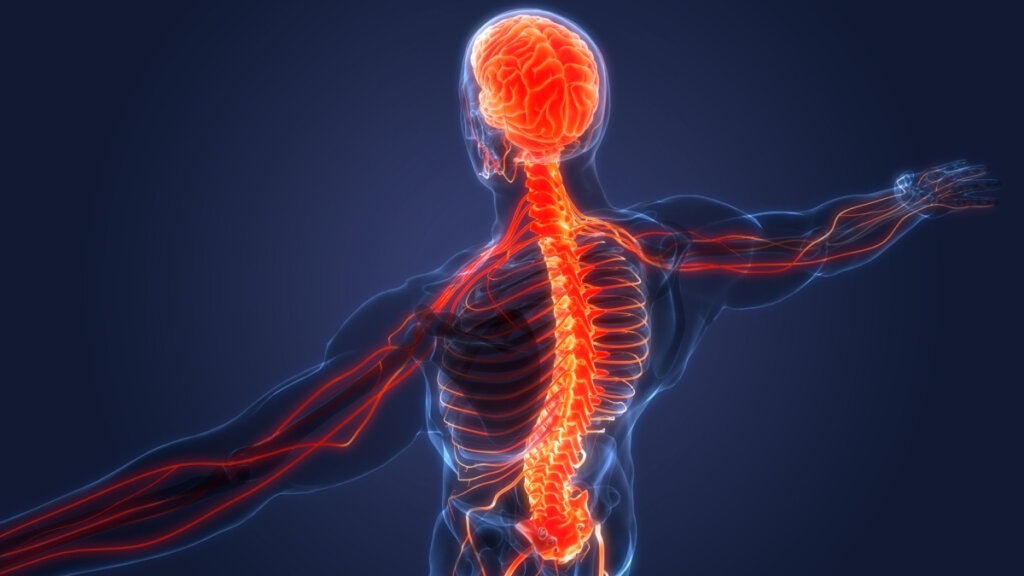
Dysautonomia is a disturbance or dysregulation in the autonomic nervous system (ANS). This system controls numerous involuntary functions of the body that are crucial for survival. For example, temperature, blood pressure, and intestinal activity. To carry this out, the system maintains a balance between the sympathetic ANS (which activates the body) and the parasympathetic ANS (which manages rest). When deficiencies occur in the regulation of these two components, the symptoms of dysautonomia appear.
The symptoms can be varied and manifest themselves differently in each individual. They usually include fatigue, dyspnea, chest pain, blurred vision, dizziness, and fainting. In addition, in most cases, orthostatic hypotension (sudden drop in blood pressure) occurs when the individual moves from sitting or lying down to an upright position.
Psychological aspects of dysautonomia
Although dysautonomia is a medical condition, at the beginning of the twentieth century, it was defined differently.
In fact, at that time, dysautonomia was known as neurasthenia or autonomic neurosis. Even today, it’s considered to be influenced by certain psychological factors that mediate ANS function. In other words, there are emotional factors that can trigger it. By identifying and working on them it’s possible to prevent and help manage this condition.
The consequences at the psychological level are usually significant right from the start. Yet, it’s often difficult for the patient to obtain an accurate diagnosis. Indeed, there’s usually a pilgrimage between different professionals who either can’t identify the illness or confuse it with other similar conditions. This lack of medical validation produces great anguish and frustration in the patient, as well as fear and a strong desire to be normal again.
Moreover, their quality of life is greatly affected. In fact, they’re barely able to stand up and experience various symptoms that, although not serious, are disabling. Consequently, their social life is greatly reduced and their close relationships are affected. In addition, it’s common for them to lose their job due to not being able to perform properly. In addition, their daily activities become increasingly restricted and they develop a sedentary lifestyle.
All of these repercussions generate high levels of anxiety and depression. In turn, they feed back and worsen the symptoms of dysautonomia.

Psychological intervention
There’s not really a cure for dysautonomia. However, multidisciplinary intervention can greatly help in the management of symptoms so it’s important that professionals from various fields join forces. The field of psychology can make a number of different contributions:
- Carry out psychoeducation in order to inform the patient about their condition and about the influence of psychosomatic factors. In effect, teach them to detect the stress factors that may contribute to the onset of their symptoms.
- Promote intelligent regulation of their emotions. Emotional self-knowledge allows them to recognize their feelings, name them, and be aware of their consequences. Likewise, they should be encouraged to recognize the virtues, resources, and tools available for facing adverse situations and promoting experiences of well-being.
- Train them in relaxation and breathing techniques. These favor the regulation of physical and psychological activation.
- Help them establish a social support network that offers them support and promotes their self-esteem. This helps them avoid isolation. They should also be encouraged to participate in rewarding activities.
- Teach them to work on any possible cognitive errors regarding the interpretation of their physiological responses. This will prevent them from developing fears and phobias that could condition their lifestyle.
- Give them guidance regarding reintegration into the labor market. It’ll help them recognize their aptitudes and interests and find an occupation that allows them to be active without exhausting themselves.
The interaction of mind and body
In short, when carrying out a holistic and comprehensive approach, the psychological aspects of dysautonomia must be considered. After all, mind and body aren’t separate. They continually interact and influence each other. This is reflected in the causes and the consequences of dysautonomia, as well as its possible treatment.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Castro, A.G., Ciallella, M.L., Linares, A.Y., Moreno, I.M., del Valle, R., & Scadding, M.D. (2016) Modelo de abordaje PNIE para disautonomía-STOP. Facultad de Ciencias Exactas, Físicas y Naturales, Universidad Nacional de San Juan. http://www.unsj.edu.ar/unsjVirtual/DiplomaturaPNIE/wp-content/uploads/2017/03/Castro_y_Otros.pdf
- González-Hermosillo, J.A. (2014). “La neurastenia de ayer, la disautonomía de hoy”, en E. Ruelas, A. Lifshitz, & G. Heinze, (Ed.) Estado del Arte de la Medicina (págs. 15-16).
- En Academia Nacional de Medicina, Estado del Arte de Medicina 2013-2014.
- Gutiérrez Herrera, C., Pizzeghello, J. P., Lucero, C., & Songer, N. (2020) Disautonomía: una patología confundida y relegada. Efectos psicosociales y propuestas de intervención psi. Facultad de Psicología, Universidad Diego Portales.
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








