Psychosis: What Is It, What Causes It, And How Do You Treat It?

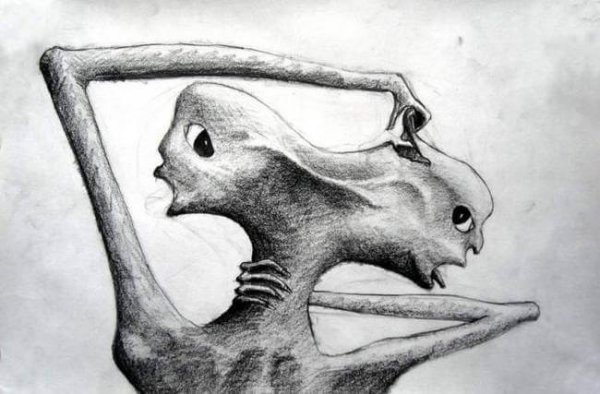
We can define psychosis broadly as: “a mental disorder in which mental functioning is sufficiently impaired as to interfere grossly with the patients capacity to meet the ordinary demands of life.” (KMLE Medical Dictionary).
If you look at this definition you might think of certain illnesses that can cause psychosis or psychotic symptoms. These range from schizophrenia, schizotypal personality disorder, psychotic disorders induced by medication or drugs, and psychotic disorders with other medical causes.
What is psychosis?
Disorders on the schizophrenia spectrum and other psychotic disorders are defined by abnormalities in one or more of the following five areas: delusions, hallucinations, disordered thought (speech), disordered or abnormal motor function (including catatonia), and negative symptoms. This is according to the DSM-V. Now, let’s look at the characteristics of these symptoms of psychosis.
Delusions
Delusions are firm beliefs that aren’t open to change, even faced with undeniable evidence that disproves them. They vary widely in subject (they could be religious, delusions of grandeur, etc).
Although it’s an over-simplification, we might call them something like “made-up stories” ill people have, though they don’t know they’re made-up. Therefore, the person expresses what they think is real and acts accordingly, even if it doesn’t correspond to reality.
We consider delusions to be eccentric if they’re clearly unrealistic, unintelligible, and don’t come from current life experiences.
- An example of an eccentric delusion is the belief that an outside force has taken away a person’s internal organs and replaced them with someone else’s, without leaving any wounds or scars.
- An example of a non-eccentric delusion is a person’s belief that they’re being watched by the police, even without any convincing proof.

Hallucinations
Hallucinations are perceptions that come about without any external stimulus. They’re vivid and clear, with all the strength and impact of normal perceptions. But they can’t be voluntarily controlled. They may occur with any of our senses, but auditory hallucinations are the most common with schizophrenia and other similar disorders.
According to the DSM-V, auditory hallucinations are most often experienced in the form of voices, familiar or unfamiliar, that are perceived as outside of a person’s own thoughts. There are also tactile, olfactory, and visual hallucinations.
Disordered thought (speech)
Disordered thought (formal thought disorder) can usually be detected in a person’s speech or way of talking. It’s very hard to hold a conversation with some people with psychosis. They might change the subject suddenly. They may respond to questions we never asked. And their speech might be so disordered it’s practically impossible to understand.
Highly disordered or abnormal motor function (including catatonia)
Highly disordered or abnormal motor function can manifest in different ways, from childish “silliness” to unpredictable agitation. A person may have trouble carrying out a task a specific goal in mind. Thus they may have difficulty doing everyday things.
Catatonic behavior appears as a marked decrease in a person’s reactivity to their environment. It may look like:
- a resistance to following instructions
- a rigid, inappropriate, or eccentric posture
- a total absence of verbal or motor responses
Other characteristics are:
- stereotyped, repetitive movements
- staring
- grimaces
- not talking at all
- echolalia (repetition of words or syllables)
Negative symptoms
Two of especially prominent negative symptoms of schizophrenia are reduced emotional expression and apathy. First of all, reduced emotional expression consists of a reduction in a person’s expression of emotions through facial expressions, eye contact, tone of voice, and movements of hands, head, and face that usually accompany our speech.
Secondly, apathy is a reduction in activities done either by personal initiative or for a specific purpose. The person might remain seated for long periods of time and show little interest in participating in work or social activities.
What causes psychosis?
This is a hard question to answer because there’s no single cause. In fact, there is a wide variety of factors or causes of psychosis. Thus, we’re going to try to answer this question by looking at the different “illnesses” psychotic symptoms can cause.
Schizophrenia
Genetic factors play an important part a person’s risk of developing schizophrenia. This is true even though most people diagnosed with schizophrenia don’t have a family history of psychosis.
Complications with pregnancy and childbirth associated with hypoxia (lack of oxygen) and older age also correlate to a higher likelihood of schizophrenia. Additionally, negative situations during pregnancy can also influence this, like stress, infection, malnutrition, gestational diabetes, and other medical conditions.
Birth season has also been linked to a higher incidence of schizophrenia. For example, in some places it’s the end of winter/the beginning of spring. The incidence rates of schizophrenia and related disorders are also higher in children who grow up in an urban environment, and in some ethnic minorities.
Schizoaffective disorder
This disorder is defined as an uninterrupted period of illness including a major emotional state episode (mania or major depression) as well as delusions, hallucinations, disordered speech, very disordered behavior, or negative symptoms.
There might be a greater risk of suffering from schizoaffective disorder for families in close contact with people who have schizophrenia, bipolar disorder, or schizoaffective disorder.
Brief psychotic disorder
Risk factors for this disorder are made up of pre-existing personality disorders and characteristics, like schizotypal personality disorder, borderline personality disorder, or specific characteristics like suspicion. Brief psychotic disorder tends to occur after a stressful incident. However, that doesn’t mean all stressful incidents lead to brief psychotic disorder.
Other psychotic disorders
In general, we can say that psychosis will not develop in a person without the necessary “certificates.” The main risk factor is biological. The trigger tends to be some sharply stressful situation in a person’s life, or using certain drugs.
While not all psychotic episodes come from taking drugs, it does increase the risk. Certain drugs, like cannabis, can lead to a psychotic episode. People who have already had an episode are especially sensitive to the harmful effects of drugs, especially if their episode was related to taking drugs.
There’s a lot of research being done about the possible causes. We’re not sure of the exact mechanisms that cause these symptoms to appear and evolve. That said, the stress-vulnerability model is the most accepted conclusion of recent research.
According to this model, a person with psychotic symptoms is more vulnerable than other people to the illness. This might be due to some biological factor or some incident in their life.

Treating psychosis
The treatment plan for a psychotic disorder has to be multidisciplinary and well-coordinated, since the therapy is normally done by multiple professionals. Recommendations for a suitable therapeutic plan:
- First, evaluation and diagnosis of the symptoms.
- Next, development of treatment plan. The preferred method of treatment is pharmaceutical, but this can also be supported with psychological therapy, which has a greater impact on negative symptoms, psychosocial functioning, cognitive functions, and specifically a person’s quality of life.
- Finding a suitable doctor/psychologist-patient relationship, where the professional takes an active interest in the treatment.
- Education about the illness for the patient and their family members.
- Treatment of other comorbidities.
- Therapy for the patient’s social functioning.
- Integration of the patient’s different treatments.
- Information on the treatments being done.
Pharmaceutical treatment
Medication is always the preferred method of treatment for psychosis patients. But this treatment is most effective when combined with psychological therapy.
Medications prescribed to these patients are antipsychotics and neuroleptics. In addition, anxiolytics and antidepressants are commonly prescribed, with end goal of treating the anxious and/or depressive symptoms.

Psychological treatments
Psychoeducational family therapy
Family therapy is fundamental; the family needs to understand the symptoms so they can manage them well. Some goals of psychoeducation are:
- giving a good explanation of the disorder
- lightening the family’s burden
- encouraging a warm family atmosphere
- improving communication
Social skills training
Most people with psychosis have a lack of social skills that contributes to relapse and worsened symptoms, on top of very low levels of social functioning. For example, a therapist will work on their:
- gestures
- verbal fluidity
- tone and rhythm of language
- posture
- expression
- emotional and social expression
Integrated Psychological Therapy (IPT) by Roder and Brenner (2007)
IPT is a behavioral treatment program for schizophrenia. It’s group-based (5-7 patients) and happens three times a week, for at least three months. There are 5 modules. They include cognitive rehabilitation (cognitive differentiation, social perception, and verbal communication). In addition, they encompass social competence training (training on social skills and interpersonal problem-solving).
To conclude, treatment for psychotic disorders is usually medication supported by psychological therapy to increase its effectiveness. Pharmaceutical treatment is very important because it helps with symptoms and restoring a person’s balance. Basically, medication fosters conditions that will allow psychological therapy to work.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
American Psychiatry Association. Manual diagnóstico y estadístico de los trastornos mentales (DSM-5), 5ª Ed. Madrid: Editorial Médica Panamericana, 2014. Tsuang, Ming T.; William S. Stone, Stephen V. Faraone (julio de 2000). «Toward Reformulating the Diagnosis of Schizophrenia». American Journal of Psychiatry 157 (7): 1041-1050.
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








