Limbic System Therapy for Healing Trauma

Written and verified by the psychologist Gorka Jiménez Pajares
Stephen Porges claims that the limbic system is the “great conductor of the orchestra of emotions.” And, he’s right. Indeed, this center constitutes an extraordinary ‘highway’ in which, sometimes, as a result of trauma, emotions such as fear, sadness, and anger can collide. This means the ’emotional accidents’ that tend to occur after trauma have the potential to destroy the human mind.
Trauma can be defined as the ‘accumulation of remarkably negative events that, repeated over time, make the victim perceive himself as defenseless and develop thoughts, emotions, and behaviors that allow him to survive, but that generate extraordinary pain’.
However, for certain organizations, such as the American Psychiatric Association, there must be a ‘life-threatening event’ in order to diagnose post-traumatic stress disorder (PTSD). That said, clinical reality suggests that less extraordinary events, but more repeated over time, are capable of producing PTSD in people. For example, being sexually abused in childhood.
“The limbic system is the place where brain chemistry mixes with emotional experience, the place where the traces of our most significant experiences are created and preserved.”
-Bessel van der Kolk-
The limbic system and its link to trauma
One of the fundamental factors in healing trauma is restoring the balance that exists between two specific areas of the brain. These are the regions specialized in ‘the rational’ (the dorsolateral prefrontal cortex) and those specialized in ‘the emotional’ (basically, the amygdala).
The goal of such restoration is for people with PTSD to achieve the “perception that they are in control of their lives” (Van der Kolk, 2020). This fact is particularly relevant since one of the effects that trauma exerts on the brain is the hyperactivation of regions specialized in emotions; the limbic system.
As a result of this hyperactivation, patients react in a disorganized way. For instance, stimuli such as light, smell, touch, or a comment can be really intense for them. They induce a state of ‘hyper alert,’ similar to what we experience when we feel imminent danger.
This occurs because, during the traumatic event, they coded such stimuli as dangerous, even though the danger may currently be non-existent.
Van der Kolk claims that overcoming trauma involves “finding access to the emotional brain”. In other words, subjecting the limbic system to therapy.
We know that the neural circuits that connect to the dorsolateral prefrontal cortex and the amygdala are scarce. However, they do connect to a third structure, the medial prefrontal cortex. This region is the core of what we know as ‘self-knowledge’. The objective of the intervention in PTSD is to restore the balance between these regions so that the patient is able to self-regulate.
“The limbic system is the emotional center of the brain, the place where feelings and impulses are born.”
-Joseph Ledoux-
Interventions for healing the limbic system
There’s a multitude of interventions for healing trauma. The available evidence suggests that the best interventions gravitate around trauma-focused cognitive therapy. This may include elements of exposure, cognitive processing therapy, and EMDR (Eye Movement Desensitization and Reprocessing). These interventions reach the highest levels of evidence (1++, or 1+) and the highest grades of recommendation (A) (Fonseca et al., 2020).
“Unhealed traumas are like time bombs waiting to go off.”
-Bessel van der Kolk-
The goal is to reduce excess activation
Although pharmacology can help in this objective, it’s well known that medication is far from curing trauma. On the other hand, it’s known that 80 out of 100 fibers in the vagus nerve transmit information from various body regions to the perceptive and executive centers of the brain.
This may indicate that the human being, having suffered a trauma, can ‘train their body’ in order to reduce hyperactivation in their brain.
To this end, both yoga and neurofeedback–based interventions have been found to be beneficial (Van der Kolk, 2020).
Furthermore, training in breathing techniques is a key element in the treatment of post-traumatic stress. This is because, when patients use these practices, parameters such as their heart rates become normalized. In effect, by normalizing their pulse through a breathing exercise (voluntarily and consciously) they’re ‘modulating’ their own parasympathetic nervous system, which is responsible for activation.
“There is no such thing as a single traumatic event. Trauma is always the result of a series of painful and heartbreaking experiences that accumulate over time.”
-Judith Lewis Herman-

Increase self-awareness
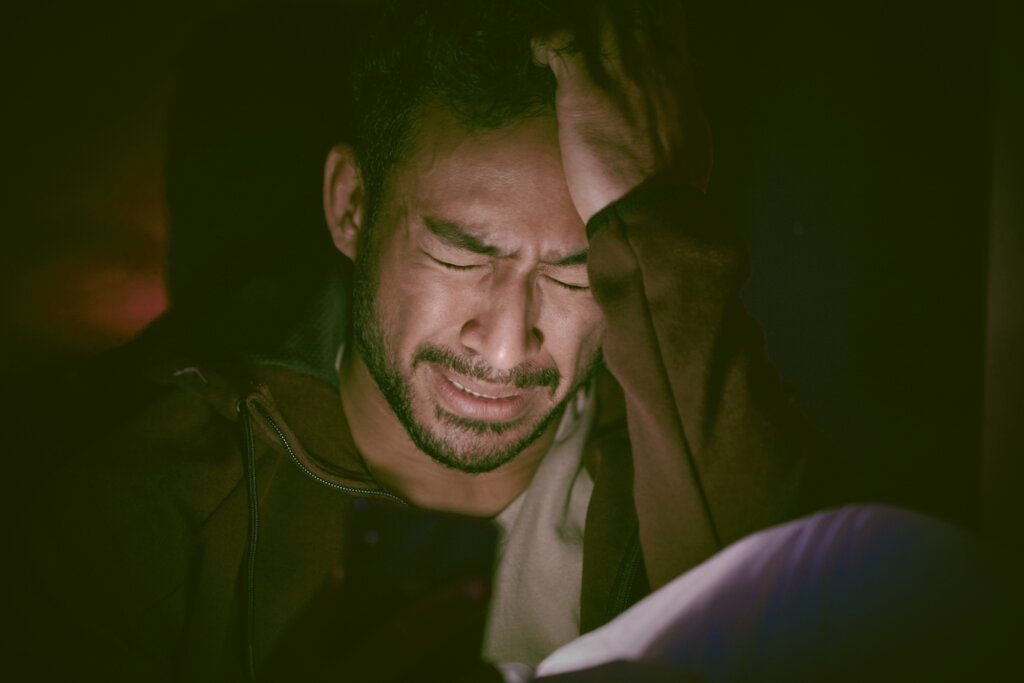
As a result of trauma, the human being can develop a phobia of emotions. In fact, the emotions they experience can be so aversive (with notable symptoms at the body level like tachycardia or a feeling of emptiness) that patients try to avoid them. As a consequence of this avoidance, their emotions increase and ‘imprison’ them in a fierce and cruel way.
Therefore, in this context, promoting techniques to increase their awareness of their emotions is essential. As a result, much research is being conducted on this issue. Benefits have been observed in mindfulness-based treatment protocols (such as MBCT and MBSR ). Among the favorable effects, it’s worth highlighting the contribution of mindfulness to the ‘extinction of fear’ (Wagner et al., 2023).
As you can see, the range of interventions to heal the limbic system and restore its balance with the ‘rational brain’ is wide. In this article, we’ve taken a brief tour of some of them and have also provided a bibliography of prestigious sources. However, healing trauma is far from simple. That said, many researchers and mental health professionals try, on a daily basis, to help their patients. They understand that, in doing so, these people are facing a real challenge.
“Traumatized people are often afraid to feel. Now, the enemy is not so much the author of the events (who, hopefully, will no longer be around to hurt them again), but their own physical sensations.”
-Bessel van der Kolk-
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- American Psychiatric Association. (2014). DSM-5. Guía de consulta de los criterios diagnósticos del DSM-5: DSM-5®. Spanish Edition of the Desk Reference to the Diagnostic Criteria From DSM-5® (1.a ed.). Editorial Médica Panamericana.
- Belloch, A. (2023). Manual de psicopatología, vol II.
- Carrobles, J. A. S. (2014). Manual de psicopatología y trastornos psicológicos (2a). Ediciones Pirámide.
- CIE-11. (s. f.). https://icd.who.int/es
- Der Kolk, V. B. (2020). El cuerpo lleva la cuenta: Cerebro, mente y cuerpo en la superación del trauma (Spanish Edition) (3.a ed.). Editorial Eleftheria S.L.
- Gesteira, C., García-Vera, M. P., & Sanz, J. (2018). Porque el Tiempo no lo Cura Todo: Eficacia de la Terapia Cognitivo-conductual Centrada en el Trauma para el Estrés postraumático a muy Largo Plazo en Víctimas de Terrorismo. Clínica y Salud, 29(1), 9-13.
- Pulido Caro, Á. P., & Barrera Aguilera, D. C. (2014). Medición de la eficacia del protocolo dunna de yoga en sujetos con trastorno de estrés postraumático (TEPT).
- Vitriol, V., Gomberoff, M., & Basualto, M. E. (2006). Relación entre trastorno por estrés postraumático de inicio tardío, abuso sexual infantil y revictimización sexual: Caso Clínico. Revista médica de Chile, 134(10), 1302-1305.
- Wagner, C., & Cáceres-Melillo, R. (2023). Mindfulness-Based Cognitive Therapy (MBCT) and Mindfulness-Based Stress Reduction (MBSR) in the treatment of Post-Traumatic Stress Disorder (PTSD): A literature review. Salud Mental, 46(1), 35-42.
- Zegarra-Valdivia, J. A., & Chino-Vilca, B. N. (2019). Neurobiología del trastorno de estrés postraumático. Revista mexicana de neurociencia, 20(1), 21-28.
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








