Learn All about Polycystic Ovary Syndrome

Written and verified by the psychologist Valeria Sabater
Living with polycystic ovary syndrome isn’t always easy. This condition is a reality for many women, even though we seldom hear of it. It manifests with pain, menstrual irregularities, infertility, and an increased risk of developing type 2 diabetes, heart disease, or depression.
It’s clear that every woman deals with this type of condition in her own specific way. However, because it was described in detail by doctors Stein and Leventhal in 1935, we know that polycystic ovary syndrome (PCOS) affects 1 out of every 10 women. We also know that many teenagers display these characteristics shortly after they begin to menstruate.
The good news is that there are better and better treatments with which to improve the quality of life of those afflicted by it. There are hormonal therapies, such as oral contraceptives added to various drugs to decrease insulin if necessary. Also, antiandrogens or dietary supplements that improve ovulation. Both of these strategies bring about good results.
It’s also important to remember the need for adequate medical supervision. In fact, many women don’t receive the diagnosis of polycystic ovary syndrome early on because they seldom go to the doctor.
Keep in mind that there’s always a disease that must receive treatment behind excessive menstrual pain, irregularities, and abnormal hair growth.
What’s polycystic ovary syndrome?

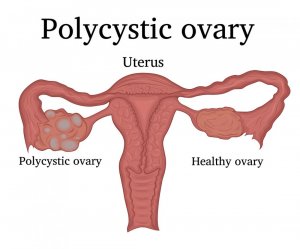
Polycystic ovary syndrome is an endocrine system disorder that affects women in their reproductive years. It’s characterized by an ovarian dysfunction, where the spent ovules aren’t always released. Instead, these thicken on the surface of the ovary, forming small benign cysts.
- The origin of this is in an alteration of androgens. Thus, to understand it better, know that ovaries produce both estrogen and progesterone.
- However, women with polycystic ovary syndrome tend to generate a greater number of androgens. This is what makes mature ovules encysting instead of freeing themselves.
These cysts aren’t malignant and don’t usually require surgery. However, they do lead to new hormonal imbalances that manifest in the following symptoms:
Anovulation in polycystic ovary syndrome
Anovulation is one of the clinical manifestations noted by women with this medical condition. It means:
- Menstrual cycles become irregular.
- There’s a lack of ovulation. This is something that afflicts half of the women with polycystic ovary syndrome. Amenorrhea or lack of period can last three months at least. Something like this leads to infertility problems, as you can imagine.
- Then, there’s metrorrhagia, another problem that usually arises. This means that some women with this problem might bleed between periods.
Hyperandrogenism
This condition responds to an alteration of the hormones where there’s an excessive level of androgens in the blood. It manifests as:
- An excess of acne and seborrhea.
- Alopecia.
- Hirsutism (the appearance of hair in unusual places in women).
Acanthosis nigricans (skin spots)
Acanthosis nigricans is a skin condition where areas such as the groins, armpits, or parts of the neck become darker and rougher. It’s a disorder that comes with its own hormonal alterations, and also with insulin resistance. In some cases, this fact can be evidenced as a side effect of some drug or contraceptive.
Illnesses associated with polycystic ovary syndrome
As we mentioned at the beginning of this article, polycystic ovary syndrome can lead to metabolic alterations. These, in the long term, lead to other relatively serious health problems. Here are some of them:
- First of all, about 50% of women with this condition can develop insulin resistance. Studies such as the one carried out by Dr. Richard Legro from the University of California, indicate that this syndrome is related to the development of type II Mellitus diabetes.
- Likewise, it’s also common to have high blood pressure. This, in turn, can lead to other cardiovascular diseases.
- In contrast, keep in mind that this medical condition is closely tied to a greater number of depression diagnoses. This is mainly rooted in self-esteem issues generated by the appearance of hair, acne and other physical disorders that affect the self-love of many young people.
Treatment for polycystic ovary syndrome
The medical approach to the polycystic ovary is multidisciplinary. Likewise, each woman will receive an individualized treatment that will start from the degree of hormonal alteration. To do this, you must follow some simple steps:
- First, you’ll need a gynecological examination with ultrasound.
- Then, a blood test to measure the concentrations of androgens, insulin, and other hormones. In this way, a physician can make a more adjusted diagnosis in each patient.
Gynecologists, endocrinologists, nutritionists, and psychologists
Any woman with this kind of metabolic syndrome undoubtedly needs a multidisciplinary approach. One in which different professionals can give her an appropriate treatment for each area that comprises this disorder. On average, the therapeutic approach integrates the following strategies:
Pharmacological
- The prescription of contraceptives to regulate ovulation.
- Also, of antiandrogens to treat hirsutism and skin conditions.
- In addition, drugs to treat insulin resistance.
Nutritional
- This is to improve diet in cases where excess weight is a problem.
- Also, to regulate hypertension and problems by using insulin.
- And, to regulate hormones and swelling.
Psychological
- Psychological help is key to improving self-esteem, anxiety problems, body image, and possible psychosexual alterations. Also, to improve any psychological problems associated with the infertility of many women, that often result from this syndrome.
To conclude, multidisciplinary assistance is vital in this type of disease. Early diagnosis will also improve the quality of life of any women with this condition, hence the importance of publicizing and normalizing this type of disease.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Meier, R. K. (2018, September 1). Polycystic Ovary Syndrome. Nursing Clinics of North America. W.B. Saunders. https://doi.org/10.1016/j.cnur.2018.04.008
- Legro, RS (2003). Síndrome de ovario poliquístico. En El Ovario: Segunda Edición (pp. 489–512). Elsevier Inc. https://doi.org/10.1016/B978-012444562-8/50030-6
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








