Cervicogenic Headaches: Very Common in Women


Written and verified by the psychologist Valeria Sabater
Pain on one side of the head and behind one eye, a stiff neck, nausea, sensitivity to light… Cervicogenic headaches are the third most common type of headaches, with a much higher occurrence in women.
It’s interesting to point out that, in the past, this condition’s existence was somewhat criticized. However, today, experts are taking it into account when diagnosing the causes of headaches. This is especially due to an important fact: many cases can become chronic.
If you suffer from headaches, you probably know that this kind of suffering is still often socially invisible. For instance, you’ve probably heard some people say “How can a headache be a reason for reduced workplace productivity?”
Despite that common perspective, primary care physicians well know the immense social and personal impact that migraines, tension headaches, and cervicogenic headaches can have on sufferers.
The AstraZeneca and Ferrer International laboratories, for instance, undertook a study that revealed an interesting statistic. Only 12 percent of the people who suffer from these conditions showed a drop in productivity for an average of three days. However, headache sufferers’ quality of life, when their condition becomes chronic, is highly affected.
For these reasons, we consider that it’s important to provide visibility to headache sufferers. We’ve all known or heard of someone who suffers from migraines, for instance. However, cervicogenic headaches aren’t as well known, despite the fact that the symptoms are very common in certain parts of the population.
It’s fitting to say that it isn’t just a simple neck ache or just another headache. Let’s take a closer look.
“The real pain is the one suffered without witnesses.”
-Marco Valerio Marcial-
Cervicogenic headaches: symptoms and causes
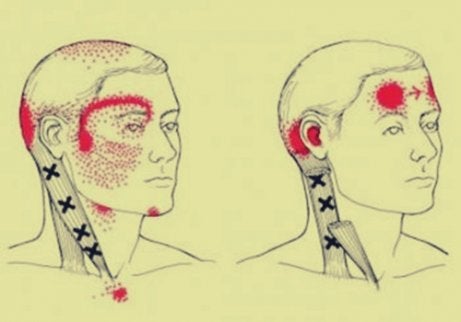
Firstly, what are cervicogenic headaches? It’s referred pain. In other words, it’s a pain that develops in the neck, though the person feels it in their head. Although it’s a headache, it has other causes such as illness or another physical issue, generally in the neck.
Studies such as this one by Toby Hall, Kathy Briffa, and Diana Hopper (2008), published in the Journal of Manual & Manipulative Therapy, show that recognition of this syndrome is growing within the medical community.
Professor Ottar Sjaastad first described cervicogenic headaches in 1993. However, it wasn’t until just a few years ago that the International Headache Society (IHS) published diagnostic information on this type of headache. They pointed to the evidence to show that this is indeed the third most common type of headache in the world.
Possible symptoms
As we mentioned above, it’s important to understand that these headaches affect women to a greater degree. A very specific fact can explain this: they’re often related to osteoarthritis. This kind of arthritis is the most common, with progressive joint wear and tear.
Now let’s take a look at some of the main symptoms of cervicogenic headaches:
- Steady pain on one side of the face, even including one eye or both.
- Neck stiffness.
- Pain when you cough or sneeze.
- Nausea and increased pain in the head when you make any movements.
- Sensitivity to light.
- Vomiting and an upset stomach.
How do cervicogenic headaches start?
Cervicogenic headaches can have different trigger points and causes. As we’ve already mentioned, one important cause is osteoarthritis (related to the C2 and C3 vertebrae). This condition can become chronic. When this is the case, the patient will need to look into therapeutic treatments that can help them have at least some quality of life.
Some of the potential causes for this condition are the following:
- Bad posture causes the joints or soft tissues to be overworked.
- Some jobs can make a person have their neck in an overextended position. The person might be unaware that they’re projecting their chin forward, not keeping their back, neck, and head straight while sitting down, for instance. This can cause stress on the neck. If the person doesn’t correct it, over time, it can lead to cervicogenic headaches.
- In addition, trauma such as whiplash or other types of injuries can also be a cause.

Treatments for cervicogenic headaches
The first essential step in these cases is to get a correct diagnosis. Many people resign themselves to believing that they’re just suffering from a simple headache. In other cases, primary care physicians may not delve deeper into the cause and may just send the patient away with anti-inflammatory tablets to treat neck or head pain.
When you have a correct diagnosis, you can look into different treatments. You may need to use several different therapies, but make sure you start with finding the original cause of the headaches. Studies such as this one by the Akershus University Hospital, in Oslo, show some different treatment strategies.
Treatment strategies
- Therapy involving back and neck exercises. The patient will do gentle exercises to relieve the pain and improve mobility.
- Physiotherapy. Massages and training by professionals specializing in treating this condition can help improve the patient’s quality of life.
- Breathing and relaxation techniques.
- Using a special pillow to make sure your head, neck, and spine are in the right position while you sleep.
- Nonsteroidal anti-inflammatory drugs are common treatment options.
- Learning to have good posture throughout the day is an essential part of avoiding this kind of headache.

Lastly, and only in the most severe cases, there’s also the possibility of surgery. This may apply to help correct compression of a nerve in the neck or spine, for instance. The cases that require surgery are limited, however, and will depend on the circumstances of each patient.
To conclude, we’d like to point out that, in the majority of cases, a combination of various different therapies and strategies can be very beneficial. Patients who are suffering from cervicogenic headaches can find relief and improve their quality of life.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Frese, A., Schilgen, M., y Evers, S. (2018). Cefalea cervicogénica. Nervenheilkunde , 37 (1), 29–32.
- Sjaastad, O., Fredriksen, TA, y Pfaffenrath, V. (1990). Cefalea cervicogénica: criterios diagnósticos. Dolor de cabeza: The Journal of Head and Face Pain , 30 (11), 725–726. https://doi.org/10.1111/j.1526-4610.1990.hed3011725.x
- O’Mullony I, Lafuente A, Pareja JA. Cervicogenic headache. Differential diagnosis and general therapeutic principles. Rev Soc Esp Dolor 2005; 12: 24-32.
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








