Multiple Sclerosis: Causes, Symptoms, and Treatment

Multiple Sclerosis (MS) is a chronic disease of the central nervous system. It exists all over the world. It is the most common cause of neurological changes in young adults and middle-aged adults, especially women.
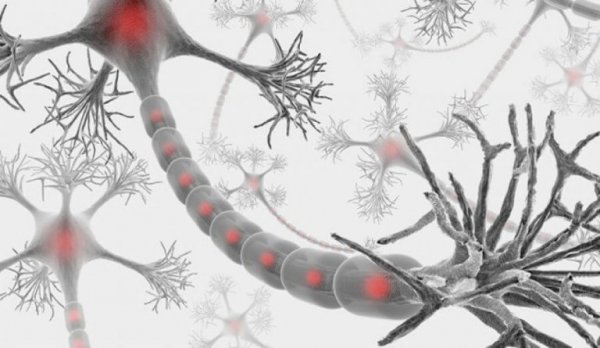
The myelin sheath is made up of proteins and fats. It protects and covers the nerve fibers of the central nervous system. Also, it facilitates the conduction of electrical impulses between the fibers.
People with multiple sclerosis have a deteriorated myelin sheath. And the deterioration can leave scars (sclerosis). Scientists also call these damaged areas demyelination plaques.
The myelin sheath doesn’t just protect the nerve fibers. It also helps them work properly. Damage to the myelin sheath drastically reduces the nerve’s ability to conduct impulses. Fortunately, damage to the myelin is often reversible.
Multiple sclerosis is an inflammatory disorder of the white matter in the central nervous system. It is characterized by multi-focal areas of demyelination, loss of oligodendrocytes, astrogliosis, and relative axonal damage.
What causes multiple sclerosis?
The etiology of multiple sclerosis is unknown. While the cause of multiple sclerosis isn’t clear, we know the disease involves several systems. Among the causes are immune and hereditary factors, as well as infections.
The exact role of viral infection in the onset and progression of the disease is unknown. Even so, scientists have studied several viruses in relation to the illness.
They relate the Epstein-Barr virus with demyelination (deterioration of the myelin sheath). There is also evidence that children exposed to the virus are more vulnerable to the disease.
Scientists have studied viruses the most out of all the environmental factors. They believe they are one of the triggering or determining factors of the disease.
Experts suspect that viruses modify oligodendrocytes during infancy. The viruses condition them to later have an abnormal immune response. Then this alters the correct myelination.
Genetic predisposition to the disease is relatively clear. Actually, studies of identical twins show that the risk of suffering from multiple sclerosis is 31%. With fraternal twins, the risk is close to 5%.
In families with multiple sclerosis, the risk of contracting the disease is 2 to 5%. The risk in the general population is only 0.1%.
Symptoms of multiple sclerosis
The onset of symptoms can be so mild that the patient doesn’t feel the need to see a doctor. The most frequent symptoms at the beginning are:
- weakness in one or more limbs
- blurry vision
- changes in sensitivity
- double vision
- difficulty coordinating movements (ataxia)
Weakness in the extremities is also common. Many people with multiple sclerosis feel fatigued when they exercise and have difficulty climbing stairs. They also lose dexterity and muscle tone. These symptoms tend to appear gradually.
Fatigue: the most common symptom
Fatigue is the most common symptom of multiple sclerosis. It affects 2/3 of patients. Half of those describe it as the worst symptom because it notably affects quality of life.
This disability is associated with depression and other factors that contribute to fatigue. Some of these are motor, limbic, basal ganglia, or hypothalamus dysfunction.
Fatigue dramatically and significantly reduces the quality of life for people with multiple sclerosis. Hence why it is so important to monitor. However, it’s difficult to manage and interpret because the perception of fatigue is subjective.
Energy loss affects motor as much as cognitive skills. We also have to differentiate between weakness, energy loss, and difficulty concentrating.
For that reason, doctors must do a differential diagnosis of multiple sclerosis fatigue with other conditions. Depression, motor disorders, thyroid problems, or side effects of anti-seizure or immunosuppressant drugs can have similar clinical features.

Flare-Ups
Flare-ups (relapses, recurrences, exacerbation) are very typical of multiple sclerosis. They are symptoms of neurological dysfunction that last more than 24 hours.
These relapses are episodes that affect distinct parts of the central nervous system and are separated by at least a month. On the other hand, when symptoms disappear, we classify that as a remission. Remission is an improvement or disappearance of signs and symptoms for at least 24 hours.
Peripheral symptoms
The following symptoms support the multiple sclerosis diagnosis when they present clinically. They are:
- L’hermitte’s Sign: the patient feels like an electrical charge is running down his entire spine. Sometimes it goes all the way to the arms or legs. Bending the neck forward triggers the sensation.
- Sensitivity to heat
- Uhthoff’s Phenomenon: increased body temperature. External factors (summer, a hot shower, smoking) or internal factors (fever, intense exercise, menstruation) can both trigger this symptom.
- Paroxysmal attacks: paroxysmal movement disorders occur suddenly and intermittently. They don’t last very long but can reappear a few times or many times a day in short bursts. The most common type of paroxysmal symptom is paroxysmal dystonia.
The progression of multiple sclerosis is impossible to forsee. However, the tendency is toward decline in physical abilities and worsening psychic and cognitive affectations.
Treating multiple sclerosis
At this time, unfortunately, there is no cure for MS. Nor is there a treatment that can positively affect the natural clinical course of the disease.
In the long term, the goal is to try to reduce the number of flare-ups. Doctors also help their patients alleviate the effects of the disease and progression of the disability.
To do this, they use immunosuppressors (azathioprine, cyclophosphamide, methotrexate) and interferons (alpha).
Doctors use high doses of corticoids for short periods of time (3-5 days) to treat flare-ups. Correctly identifying the flare-up is key to making a diagnosis and finding the correct treatment.
The symptomology of a flare-up is one or several lesions caused by an inflammatory process. That process is located in the central nervous system. And corticosteroids are the drug of choice for flare-ups because they target inflammation.
Treating the symptoms of MS
We can summarize symptomatic treatment as the following:
- Spasticity: baclofen, diazepam, dantrolene sodium…
- Fatigue: amantadine, modafinil, methylphenidate…
- Pain: carbamazepine, phenytoin, gabapentine, pregabalin…
- Bladder hyperreflexia: oxybutynin, bethanechol…
- Cognitive Deficiency: donepezil, interferon beta, memantine…

Rehabilitation
Rehabilitation is extremely important. The fundamental goal is to prevent disability in the patient. Or, at the very least, reduce it as much as possible.
Therapists teach the patients to learn new skills and maximize their healthy systems. That way they will be able to maintain a certain independence.
It is also vital to adapt or modify their social and work environments. In addition, psychological support of the patient, family, and caregivers is essential.
Experts recommend a multidisciplinary rehabilitation treatment tailored to the individual. People suffering from MS can improve their quality of life in terms of health and ability to perform day-to-day activities. In fact, many organizations for people with MS offer these types of treatments focused on holistic rehabilitation.
Bibliography
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








