What Happens to My Brain When I Have Alzheimer's?
Sad as it is to say, we are all used to hearing about different kinds of dementia, but we often do not receive clear explanations of what is happening to a brain suffering from it. For that reason, the goal of this article is to explain,in the simplest way possible, what is happening to a brain that has been diagnosed with Alzheimer’s disease.
Moreover, I will include one of the most recent and most hoped for advances in terms of treating Alzheimer’s. This advance, which was recently published by the journal Nature, is so important that its results may change the course of Alzheimer’s disease as we know it.
The brain with Alzheimer’s dementia
When someone is affected by Alzheimer’s disease, a serious degeneration of the brain takes place, particularly in the hippocampus, the entorhinal cortex, the neocortex (especially the association cortex in the frontal and temporal lobes), the basal nucleus, the locus coeruleus, and the raphe nuclei.
But what is all of this? These are different areas of the brain that, explained in the simplest way possible, are involved in the process of learning, memory, and emotional regulation. As you can see, all of these functions are strongly affected in patients with Alzheimer’s.
And how do these areas degenerate? Well, with the development of amyloid or starchy plaques and neurofibrillary tangles. However, before explaining what these plaques and tangles are, we have to know the parts of a neuron:
- Soma: this is the body of the neuron, where its nucleus is located and where the information that each neuron receives from others around it is stored.
- Axon: this is the largest projection that comes off of the soma and serves the purpose of sending information from one neuron to others.
- Dendrites: these are the small extensions that come off the body of the neuron and receive information from other neurons.
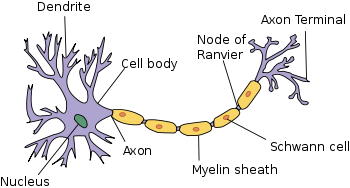
The amyloid plaques are deposits that are located outside of brain cells, made up of a nucleus whose protein is called amyloid-beta. These deposits are surrounded by axons and dendrites that are degenerating. This degeneration process is natural in every human brain; it is not pathological.
Furthermore, connected to them are activated microgliocytes and reactive astrocytes, which are cells that play a role in the destruction of harmed cells. The so-called phagocytic neurgliocytes also play a role. These are responsible for destroying degenerated axons and dendrites, leaving nothing but a nucleus of amyloid-beta.
The neurofibrillary tangles are made up of neurons in the process of going extinct and which contain intracellular accumulations of strands interwoven with tau protein. The normal tau protein is a component of the microtubules, which supply the cell’s transport mechanism.
Throughout the evolution of Alzheimer’s disease, an excessive number of phosphate ions attach themselves to the threads of the tau protein, thereby changing its molecular structure. This structure turns into a series of anomalous threads that are observed in the soma and in the dendrites closest to the cells of the cerebral cortex.
Ions alter the transport of substances within the cell, such that it dies, leaving behind a tangle of protein threads.
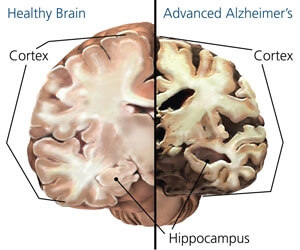
Just a second, didn’t you just say that the neurons are degenerating? Yes, and this is something that happens during the normal aging process. But in the case of Alzheimer’s disease, the formation of the amyloid plaque is due to the production of a defective sort of amyloid-beta, which sets off neuron death, thus differentiating it from normal aging.
In other words, we all have a level of plasticity in our brains; neurons that are degenerating but this does not cause any harm. They are replaced by others without us even noticing their absence.
The importance of the new treatment for Alzheimer’s
The journal Nature recently published an article entitled Alzheimer’s disease: Attack on amyloid-β protein. The main author of this article, Eric M. Reiman, goes into detail about the discovery of new advances in the treatment of Alzheimer’s, concretely, the amyloid-beta protein.
Reiman and his collaborators looked into a new drug that avoids the destruction of the neurons and accumulations of plaque from the amyloid protein, which, as we explained above, is considered one of the primary causes of the cognitive deterioration associated with Alzheimer’s.
Félix Viñuela, a neurologist and researcher at the Hospital Virgen Macarena in Seville, Spain, says that “this drug travels to the brain, attaches itself to the deposit of that toxic substance, and starts removing it from there.” Furthermore, “we have proven that the higher the dosage of this new drug we administer, the greater the recovery we see in our patients.”
However, the researchers themselves emphasize that, right now, this is a study that is being conducted at 300 hospitals in North America, Europe, and Asia, particularly with patients suffering from Mild Cognitive Impairment (MCI) and that although this is a very hopeful advance, there is still a long way to go before it can be put into practice and before they can prove its long-term effects.
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








